Choosing between surgery and radiation for prostate cancer? Our urologists provide expert insights for informed decisions at Advanced Urology Institute.
Continue readingTalking With Your Doctor About Enlarged Prostate
You are a man and, like most men, you aren’t that comfortable talking about your health. But if you live long enough or desire to live that long, you’ll have to talk about your health with your doctor. And later in life you are likely to have benign prostatic hyperplasia — about 80 percent of men will have BPH in their lifetime — and will need a urologist to either diagnose or confirm that you have the condition and then treat it.
What is BPH?
BPH means the prostate gland has grown so large that it is causing urinary problems. Often, as the gland enlarges, it presses on the urethra, narrowing or blocking it and making it difficult for urine to pass through the tube. Eventually BPH may cause bothersome and embarrassing urinary symptoms that may require specialized treatment.
You should see a urologist when:
- You are finding it problematic to start to urinate.
- You frequently have a sudden, uncontrollable urge to urinate.
- You have dripping or leaking of urine after you urinate.
- You have weak, slow or interrupted urine streams.
- You urinate frequently, particularly at night.
- You experience pain or discomfort or have to strain or push to urinate.
- You can’t empty your bladder completely.
Why should you see a urologist?
BPH should be promptly treated by a urologist because it can have adverse effects on your life. The condition can lead to complications such as urinary tract infections, kidney failure or urinary retention. Likewise, BPH may reach a point where you may have to plan every errand, activity or event you are attending around its proximity to a bathroom.
You also should see a urologist if you have a family history of the condition. The doctor will guide you on the actions to take to prevent or manage the condition, helping you avoid complications and make treatment more cost-effective. And since BPH and prostate cancer may have similar symptoms, speaking with your doctor about your symptoms may help you detect a more serious condition earlier.
How should you speak with a urologist?
Most problems brought to urologists are embarrassing. So rest assured that talking about BPH with the doctor is not a shameful, intimidating act but a courageous, lifesaving step. Don’t be reluctant to open up. Be willing to talk freely since the condition has a great prognosis if treatment begins early. Also there is a lot of value speaking with a urologist when the symptoms are still at their mildest stage because only a simple intervention may be needed. It is important to seek help as soon as symptoms begin to occur.
You should come to your appointment prepared with your complete medical history, medications and all the relevant information about your health and the procedures you have had in the past. You also should bring any information about your condition and a list of questions to ask.
Once you’re at the urologist’s office, make sure you are completely honest about the reasons for your appointment. Be open and say you are visiting because of your urinary problems. Honesty will help to prepare you and the entire urology team that will handle the case. It is also critical to talk about all the changes that you have seen in your health.
While treatment for BPH can be as simple as just avoiding alcohol and caffeine, emptying your bladder as completely as you can, or taking prescribed medication to reduce the symptoms, prevent further growth of the prostate or shrink the prostate, your primary focus should be on achieving an improved quality of life after treatment. Ask the urologist about the possible side effects of the potential treatments, the right treatment for you and how comfortable it will be for you moving forward. Whenever possible, seek non-surgical interventions first before you consider surgery.
If the condition can’t be controlled with medication, such as in severe BPH or when you have complications like bladder stones, urinary tract blockages or kidney problems, your doctor may suggest surgery. Various forms of surgery include laser therapy, transurethral prostatic incision, needle ablation or microwave therapy. It is important to speak with your urologist about the different surgical options before you are treated. For more information on diagnosis and treatment of BPH, visit the “Advanced-Urology-Institute‘” site.
Can females see a urologist?
There is a misconception that urologists only see male patients. In fact, over 40 percent of patients seen by urologists are female. Urologists are specialists in treating disorders of the urinary tract — the system of tubes, muscles and organs that process, convey and eventually expel urine from the body. So when women develop urological issues, such as loss of bladder control, pelvic organ prolapse and incontinence, the best doctor to treat them is the urologist. Warning signs of issues involving the urinary system include:
- 1. Frequent urge to urinate.
- Leaking urine.
- Frequent urination, particularly at night.
- Pain in the side or back.
- Discomfort or burning sensation when urinating.
- Pelvic pain
- Blood in urine
Apart from treating kidney stones, urologists frequently tackle the following issues in women:
1. Loss of bladder control
 Females may have bladder control problems at any age. Also called urinary incontinence (UI), loss of bladder control is a common problem in women and they are twice as likely to have the problem as men. There are different types of urinary incontinence. For example, women who can’t hold urine as they cough, sneeze or exercise are said to have stress incontinence. This type of UI occurs when the muscles supporting the bladder are weakened by pregnancy, childbirth, aging or other factors.
Females may have bladder control problems at any age. Also called urinary incontinence (UI), loss of bladder control is a common problem in women and they are twice as likely to have the problem as men. There are different types of urinary incontinence. For example, women who can’t hold urine as they cough, sneeze or exercise are said to have stress incontinence. This type of UI occurs when the muscles supporting the bladder are weakened by pregnancy, childbirth, aging or other factors.
Overactive bladder is another type of urinary incontinence that is characterized by a strong, sudden and uncontrollable urge to urinate even when the bladder is not full. Apart from the need to reach the bathroom quickly and to pass urine 8 or more times within 24 hours, overactive bladder can cause embarrassing urine leaks and compel women to avoid certain activities and things they would like to enjoy.
2. Recurrent urinary tract infections
Women are more susceptible to recurrent urinary tract infections than men because of anatomical differences. Most women will have a urinary tract infection at a certain point in their lives. The infections occur when bacteria get into the urinary tract and are often characterized by burning sensation or pain during urination, sudden urge to pass urine, blood in urine or trouble urinating. Recurrent UTIs can lead to complications and require prompt, proper treatment.
3. Fallen bladder
In women, the bladder is kept in position by tissues called pelvic muscles. But in cases where these tissues (wall between bladder and vagina) are too stretched or weakened to hold the bladder in position, the bladder may fall into the vagina — a condition known as bladder prolapse or cystocele. A fallen bladder may be caused by aging, childbirth, lifting heavy objects, menopause, chronic coughing, obesity or previous pelvic surgery, and may lead to urinary incontinence, urinary tract infections or overactive bladder if not treated. Surgery is typically required to correct a fallen bladder.
4. Painful bladder syndrome
Also called interstitial cystitis (IC), painful bladder syndrome is an uncomfortable and upsetting condition accompanied by lower belly and bladder discomfort. Patients tend to feel that their bladder is always full and often feel the urge to pass urine several times per day, even up to 60 times in one day. The condition can badly interfere with daily activities, forcing affected women to avoid traveling far away from home and to skip social events. It also can make sex painful or uncomfortable.
As urologists, our job is to figure out what kind of bladder problem a woman has, its underlying cause and the appropriate treatment for it. With the right treatment, which may include pelvic muscle strengthening exercises, medication, injections, implanted devices and surgery, most women are able to regain their bladder control and recover from their condition. And even for conditions that have no cure, such as interstitial cystitis, treatment tends to ease symptoms and boost the quality of life.
At Advanced Urology Institute, we see women with many different urological issues. Our aim is always to help them enjoy life and all activities they’d want to engage in by eliminating awkward urine leaks and the pain and discomfort associated with these conditions. If you are a woman who is tired of having embarrassing accidental urine leakage, check with us about effective treatment. For more information on the diagnosis and treatment of urological issues in women, visit the “Advanced Urology Institute” site.
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
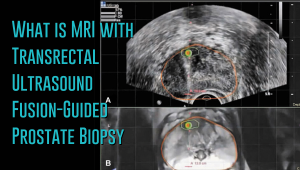 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Diagnosis and Treatment of Urologic Cancer
Diagnosis of urologic cancers
Diagnosis of urologic cancers usually starts with symptoms, although some patients don’t show symptoms and their tumors are detected during routine imaging. At AUI, our approach to cancer diagnosis includes patients’ symptoms, personal medical history, family medical history, physical examination, screening and diagnostic testing. The symptoms of urologic cancers tend to vary with the type and location of the tumor, but may include abdominal pain, blood in urine, elevated hormone levels, swollen abdomen and enlarged prostate. In terms of diagnostic tests, we often use biopsy, blood tests for hormone levels, digital rectal exam, liver function tests, pelvic exam, renal arteriography, bone scan, ultrasound, urine test, CT scan and MRI scan.
Care after cancer diagnosis
 At Advanced Urology Institute, we understand that diagnosis with urologic cancer is shattering and distressing. So we speak with our patients soon after diagnosis to bring their emotions under control and give them hope. For us the goal is not just to cure cancer but also to prepare and help our patients to face the challenges that may come with the disease. That’s why we work collaboratively with clinicians, researchers, dieticians, nurses, radiotherapists, radiologists and other medical professionals to ensure optimal outcomes are achieved with minimal impact on our patients’ quality of life.
At Advanced Urology Institute, we understand that diagnosis with urologic cancer is shattering and distressing. So we speak with our patients soon after diagnosis to bring their emotions under control and give them hope. For us the goal is not just to cure cancer but also to prepare and help our patients to face the challenges that may come with the disease. That’s why we work collaboratively with clinicians, researchers, dieticians, nurses, radiotherapists, radiologists and other medical professionals to ensure optimal outcomes are achieved with minimal impact on our patients’ quality of life.
Treatment of urologic cancers
We follow a multidisciplinary approach when treating urologic cancers. That means a wide-range of certified medical experts evaluate a patient’s condition and develop a comprehensive, personalized treatment plan depending on the type, stage and location of the cancer and the patient’s overall health. In a number of cases, surgery may be the primary treatment for urologic cancer and we provide minimally-invasive laparoscopy, robotic surgery, percutaneous cryosurgery and reconstructive procedures that deliver optimal outcomes with reduced scarring, less pain and shorter recovery time. Every patient’s candidacy for surgery is evaluated after diagnosis or during first appointment, but we are always confident of taking on some of the toughest cancer cases and striving to provide the best surgical outcomes and patient experience.
AUI also provides a number of advanced urologic cancer therapies. We offer current and investigational treatments and provide advanced radiation therapies including prostate brachytherapy (radiation seed implants). Treatment options for urologic cancer may include chemotherapy, hormone therapy, immunotherapy and radiation therapy. For instance, we deliver targeted regimens of radiation that are sculpted to the shape and size of the tumor ensuring that their impact is focused on cancer cells while limiting exposure of adjacent normal tissues. Likewise, urinary diversion techniques, fertility-preserving options and drugs with fewer side effects are prioritized. And with our extensive team of survivorship and supportive care experts, who help patients and their caregivers to attain and maintain a better quality of life before, during and after treatment, we often achieve great outcomes for our patients.
Recognized leader in care for urologic cancers
Advanced Urology Institute has a urology oncology team that is a nationally recognized leader in the management of urologic cancer. We have state-of-the-art equipment, leading urologists in their field and imaging and pathology experts who are good at what they do. What that means is that our patients get the best possible care at every stage of their journey with cancer. We manage urologic cancers in an outpatient setting, allowing our patients to go home the same day. And when they go home early from our day cancer center, we monitor them very closely. We are proud that, in most cases, our cancer patients do really well.
At AUI, our goal is not just to cure cancer but also to prevent it from spreading and from coming back. We are also committed to working with the local communities and spreading the word for people to get tested early. For more information on the prevention, diagnosis and treatment of urologic cancers, visit the “Advanced Urology Institute” site.
Kidney Stone Causes, Symptoms, and Treatments
Symptoms of kidney stones
At Advanced Urology Institute, we see a lot of patients with kidney stones. A contributing factor is our location in Florida, with its massive heat and humidity which leads to dehydration and, unfortunately, to the formation of these painful stones in the kidneys. The stones commonly present with severe, intense pain — like something is stabbing you — and you can barely walk. Kidney stones are characterized by sharp pains in the side or back as they make their way to the bladder. Most of our female patients usually say the stones are more painful than labor pain. Other symptoms of kidney stones include vomiting, nausea, a constant urge to pass urine and blood in urine.
Pain from kidney stones is often sudden in onset, though it may get severe over a period of hours in some cases. The pain may be either intermittent (colicky) or steady and, depending on the stone’s location as it moves through to the bladder, it may begin in the back or flank area and radiate slowly downward to your inguinal ligament, urethra, bladder, testicles or penis. Urinary or bladder symptoms, such as frequency of urination and painful urination, may occur if the stone is located in the portion of your urethra found within the bladder wall. Not all stones cause pain and some of them are often discovered “incidentally” during pelvic or abdominal X-rays. But in patients who experience pain, they usually describe it as the worst pain they have ever experienced.
Diagnosis of kidney stones
Diagnosis of kidney stones is almost entirely based on the history of passing the stones or on occurrence of a stabbing pain in the side or back. We usually place emphasis on the patient’s clinical signs, familial disorders, presence or absence of any previous renal stones, or physical exam findings. We also perform a urinalysis to check the presence of white cells (pyuria) or blood (hematuria) in urine, a culture of urine to exclude infection, and use the presence of crystals in urine (crystalluria) to help identify the stone type. Patients are often required to strain their urine to obtain the stone for crystallographic analysis. Analyzing kidney stones for their mineral composition helps us understand your future risk and to recommend the right dietary habits and restrictions for preventing stones. But we also do a CT or CAT scan of the pelvic and abdominal area to evaluate the size, location, degree of hydronephrosis and density of the stone, all of which are important in determing how we treat and manage the stones.
Treatment
When patients complain of symptoms of kidney stones, we usually do physical exams and run tests to confirm that they actually have stones. But we often begin by getting the pain under control and calming the patients, to enable us to discuss with them available treatment options. The pain due to kidney stones is relieved using pain medication, drinking plenty of fluid to prevent dehydration, and ordering bed rest. In many cases once we have assessed that the stones can pass on their own, we allow about 7 days for them to pass spontaneously. In other instances, however, kidney stones may need to be broken down into tiny pieces or to be removed surgically.
At Advanced Urology Institute, we break up kidney stones using such techniques as percutaneous lithotripsy, cystoscopy or extracorporeal shock-wave lithotripsy. For renal stones less than 2cm in size, we generally treat them using extracorporeal shock-wave lithotripsy. During the procedure, high-intensity ultrasound (shock-waves) are passed through pouches of water placed on the skin and then directed toward the stone. The waves break the kidney stones into tiny pieces that can pass easily through the ureter. For stones located higher in the ureter or in the bladder, we often use cystoscopy to pull them out or break them up with electric energy or laser. During the procedure, the doctor passes a viewing tube with a crushing device into the ureter or bladder to pull the stone out or break it up with electric energy or laser.
For larger stones, percutaneous nephrolithotomy is a safe and reliable technique. For this procedure, you’ll be given medication to sedate you, then a viewing tube will be inserted through an incision made in your side. Once the stone is reached, it’s broken up using electric energy or ultrasound. In cases where this procedure doesn’t work, particularly when the stones are hard to reach or too large, surgery is often the preferred treatment. Surgery to remove kidney stones is performed under general anesthesia with the doctor making an incision into the side and another into the kidney or ureter to remove the stone. After the stone is removed, the incisions are stitched up.
There are many ways of treating kidney stones and the method chosen usually depends on the experience and judgment of the urologist, together with the patient’s preferences. At AUI, we prioritize the comfort of our patients, so we opt for the least invasive procedures before considering surgery. Want to know more about prevention, diagnosis and treatment of kidney stones? Find more information from the “Advanced Urology Institute” site.