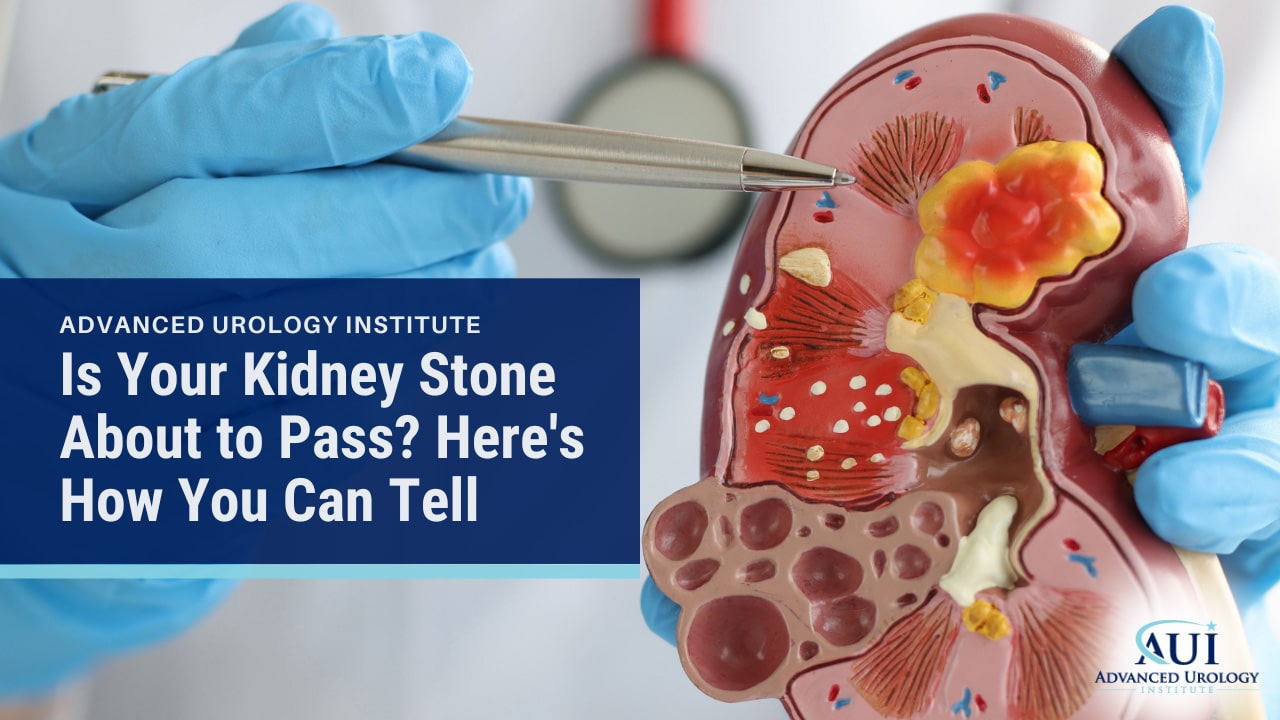
How can you tell if your kidney stone is about to pass? Learn to see the signs that can bring some predictability to an otherwise painful process.
Continue readingAdvancement In Technology Helps in Prostate Cancer Radiation Therapy
The Advanced Prostate Cancer Institute in Oxford, FL is committed to the continuous evolution of prostate cancer radiation therapy.
Continue readingThe Impact of Radiation Therapy in Urological Care
Our urologists in Naples and Largo, FL provides a foundation for understanding the impact of radiation therapy in the realm of urology.
Continue readingUnderstanding Advanced Prostate Cancer with Chelsie Ferrell, PA
Chelsie Ferrell, physician assistant in Orange City, FL talks about the importance of understanding advanced prostate cancer.
Continue readingThe Importance of the PSA Test: A Key to Prostate Health
Understand the importance of the PSA test. It is recommended for men between the ages of 55-70 who expects to live at least another 10 years.
Continue readingHoward Epstein, MD: Exploring Vasectomy
Exploring vasectomy and the full implications is crucial when making the decision to have the surgery says Dr. Epstein of St Augustin, FL.
Continue readingNicole Szell, DO: Elevating Quality of Life Through Urological Expertise
Dr. Nicole Szell, a urologist in Advanced Urology Institute in Largo, FL whos demeanor and urological expertise helps her patients be at ease.
Continue readingThe Best Place for Treating Prostate Cancer in Oxford, Florida
Key Takeaways:
- The Advanced Urology Institute in Oxford, FL is a beacon of hope for prostate cancer patients, offering a collective of experts and state-of-the-art treatments.
- The institute’s presence of 25 urologists and a radiation oncologist signals the breadth and depth of their medical competence.
- Beyond the medical expertise, the institute offers holistic care with empathetic support and monthly support groups.
 When grappling with prostate cancer, there’s no such thing as a routine case. The journey involves not only physical challenges, but emotional and logistical ones as well. For those seeking treatment in Oxford, Florida, the journey may be a little less daunting. The village of Sanibel is home to a game-changing player in the world of urology. Advanced Urology Institute has positioned itself as a gold-standard provider of care. Its Oxford office is more than just a medical facility—it’s a hub of knowledge, support, and state-of-the-art treatment for those battling prostate cancer.
When grappling with prostate cancer, there’s no such thing as a routine case. The journey involves not only physical challenges, but emotional and logistical ones as well. For those seeking treatment in Oxford, Florida, the journey may be a little less daunting. The village of Sanibel is home to a game-changing player in the world of urology. Advanced Urology Institute has positioned itself as a gold-standard provider of care. Its Oxford office is more than just a medical facility—it’s a hub of knowledge, support, and state-of-the-art treatment for those battling prostate cancer.
A Collective of Experts
“My name is David Bussone and I live in the village of Sanibel here in The Villages. Well, we’re very lucky to have a facility like this. I mean, we have 25 urologists, something like that, here in this building and in other suites,” shares David, a local resident, underlining the scope of expertise available.
A collective of 25 urologists is no small feat. This commanding presence of urology specialists under one roof signals the breadth and depth of their medical competence. Regardless of your specific needs or the stage of your prostate cancer, there’s a specialist equipped to handle your case.
The Radiant Beacon: Oxford Radiation Center
“We have the radiation center here. We have Dr. Chancellor, who’s the radiation oncologist,” David notes, highlighting another crucial section of the office—the Radiation Center.
Being able to access state-of-the-art radiation therapy in Oxford, FL, is a major advantage for patients. Having access to advanced treatments within local proximity alleviates the logistical stress of traveling for care. The presence of Dr. Chancellor, a radiation oncologist, further solidifies the office’s standing as a comprehensive source of prostate cancer treatment.
A Haven of Comprehensive Care
David goes on to praise the seamless integration of services. “And just to have all of that capability and professional staff and knowledge in one location is fabulous. Everything from the staff that you see in the doctor’s office to the physicians, the urologists.”
In addition to the top-tier medical care, patients also receive unwavering support throughout their treatment journey. As David details, “They have support groups that meet here on a monthly basis.” This subtle yet significant detail underscores the holistic approach to care at the Advanced Urology Institute.
“It’s just so neat to have everything in one place. I can’t tell you how lucky we are to have something so close by,” David admits, echoing the sentiments of many who have sought treatment at the Oxford office.
A Beacon of Hope for Prostate Cancer Treatment
Oxford, FL, is endowed with an invaluable asset in the Advanced Urology Institute. This isn’t just a urology practice; it’s a beacon of hope for prostate cancer patients. With its collective of experts, advanced treatments, and empathetic support, it has set a new standard for urology care in Florida.
The institute’s commitment to delivering exceptional care has earned it the distinction of being the largest urology practice in Florida. But beyond the numbers, it’s the life-changing impact on patients that truly defines their success. For anyone faced with the daunting challenge of prostate cancer, the Oxford office offers a sanctuary where battle-tested expertise meets unwavering compassion in the quest to beat prostate cancer. So, for those in need, remember, the Advanced Urology Institute in Oxford, FL, is more than just a place; it’s a partner in your journey to healing.
References:
- Prostate Cancer | Advanced Urology Institute. (2023, September 26). Advanced Urology Institute. https://www.advancedurologyinstitute.com/conditions-we-treat/prostate-cancer/
- Advanced Urology Institute. (2023, September 19). Patient’s Satisfaction is #1 At Advanced Prostate Cancer Institute. Advanced Urology Institute. https://www.advancedurologyinstitute.com/patients-treatment-and-satisfaction-is-1-at-advanced-prostate-cancer-institute/
- Advanced Urology Institute. (2023, September 12). What Technologies Are Used in Advanced Prostate Cancer Institute. Advanced Urology Institute. https://www.advancedurologyinstitute.com/what-technologies-are-used-in-advanced-prostate-cancer-institute/
- CDC. (2023, July 17). How Is Prostate Cancer Treated? Centers for Disease Control and Prevention. https://www.cdc.gov/cancer/prostate/basic_info/treatment.htm
- Health, U. (2023, January 31). Radiation Therapy for Prostate Cancer. Ucsfhealth.org; UCSF Health. https://www.ucsfhealth.org/treatments/radiation-therapy-for-prostate-cancer
- Radiation Therapy for Prostate Cancer. (n.d.). Www.cancer.org. https://www.cancer.org/cancer/types/prostate-cancer/treating/radiation-therapy.html
What Causes Erectile Dysfunction and How Can It Be Cured?
Key Takeaways:
- Erectile dysfunction is a persistent difficulty in achieving or maintaining an erection, firm enough for satisfactory sexual performance.
- The causes of ED are multifaceted, with physical, psychological and medical factors contributing.
- Treatment options range from lifestyle changes to medications, penis pumps, surgery and implants, as well as psychological therapies. Seeking help from a healthcare professional is essential.
You may see the term ‘erectile dysfunction‘ (ED), also known as impotence, slipped into the hushed conversations of men, or used as the punchline of a far too common bathroom joke. Your neighbor, your hairdresser, even your favorite sitcom — they’ve touched on it. But, do you truly understand what ED is? More importantly, do you realize that it’s a topic that deserves open conversations and thorough understanding?
Defining and Understanding Erectile Dysfunction
Simply put, erectile dysfunction is a persistent difficulty in achieving or maintaining an erection, firm enough for satisfactory sexual performance. It’s not an aphrodisiac dinner conversation, granted. Yet, understanding its causes and treatment options can help those affected to regain their potency, self-esteem, and quality of life.
The Triggers Behind Erectile Dysfunction
Like a complex puzzle, the causes of ED are multifaceted. Physical factors are substantial contributors. Medical conditions such as diabetes and hypertension can cause ED. Hormonal imbalances and neurological disorders, too, can curb your virile enthusiasm. Meds for other ailments or substance abuse may also inadvertently set the stage for ED.
Meanwhile, psychological factors should not be overlooked. The ever-dreaded performance anxiety can lead to ED, as can stress and strains in relationships. Depression and other mental health conditions could also provoke these sexual malfunctions. It’s like a minefield, with triggers at every turn. But, don’t despair. There are ways to navigate it.
How to Treat Impotence
Firstly, lifestyle changes are beneficial. Adopt a healthy diet and exercise regime. If you smoke, it’s time to stub it out. Consider reducing your alcohol activity — moderation is the key. Learn stress management techniques to help defuse those potential ED time bombs.
Medications such as Viagra and Cialis can work wonders. Injectable medications can also be an option. If your doctor decides to pull out the big guns, penis pumps, surgery, and implants may be suggested.
Penis pumps and vacuum erection devices are non-invasive methods, while penile implants offer a more permanent solution. Yet, these methods should be considered alongside the potential risks and side effects.
Sometimes, unraveling the psychological knots could be the key to impotence relief. A therapeutic approach involving counseling, cognitive-behavioral techniques, or both, could be proposed.
Get Professional Help
All these solutions underline the importance of a proper consultation with a healthcare professional. Urologists and sexual health specialists have the knowledge and resources to guide you through the obstacle course that is ED. They help you understand, cope, and conquer.
A Helping Hand from Advanced Urology Institute
As you howl at the ED wind, there’s a beacon poised to guide you. The Advanced Urology Institute, the most extensive urology practice in Florida, is filled with urologists in FL who are eager to help. They house specialized professionals and cutting-edge procedures to address erectile dysfunction effectively.
In conclusion, overcoming erectile dysfunction is not as daunting as it may seem. Its causes, although numerous, can be identified and managed effectively. Various treatment options from lifestyle changes to surgeries are available. The crucial factor is the willingness to seek help and adopt a holistic approach to treatment. With adequate support from distinguished institutions like the Advanced Urology Institute, victory against ED isn’t just possible, it’s probable.
References:
- Erectile Dysfunction | Advanced Urology Institute. (2023, September 19). Advanced Urology Institute. https://www.advancedurologyinstitute.com/conditions-we-treat/erectile-dysfunction/
- Advanced Urology Institute. (2019, December 13). Erectile Dysfunction Treatment Options | Advanced Urology Institute. Advanced Urology Institute. https://www.advancedurologyinstitute.com/erectile-dysfunction-treatment-options/
- And, D. (2023, September 25). Symptoms & Causes of Erectile Dysfunction. National Institute of Diabetes and Digestive and Kidney Diseases; NIDDK – National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/symptoms-causes
- Nall, R. (2015, March 12). 5 Common Causes of Impotence. Healthline; Healthline Media. https://www.healthline.com/health/erectile-dysfunction/common-causes-impotence#takeaway
- Erectile dysfunction. (2020). Nhsinform.scot. https://www.nhsinform.scot/illnesses-and-conditions/sexual-and-reproductive/erectile-dysfunction-impotence
Brian Hale, MD: Choosing Excellence with Advanced Urology Institute
Key Takeaways:
- Small medical practices are increasingly having difficulty staying competitive in the current market, leading many physicians to a crossroads between becoming an employee or merging with more doctors in their specialty just like Advanced Urology Institute.
- Dr. Hale chose to merge with the Advanced Urology Institute to augment his resources and negotiate contracts from a more competitive pedestal.
- By joining forces with Advanced Urology Institute, Dr. Hale has been able to pursue a shared vision for excellence and dedication to patient care.
As a nation, we have always cherished the tales of those individuals who choose to tread the path often left unexplored, who dare to mold their destiny according to the dictates of their integrity rather than bend to the whims of circumstances. Today, we bring to the forefront one such individual — Brian Hale, MD, a board-certified urologist serving the areas of Palm Harbor, Tampa and New Port Richey in Florida.
Shaping His Own Journey
Dr. Hale’s journey in the field of urology began in a time when solo practitioners and small practices were the norm in the profession. “When I first started urology,” he says, “there were a lot of solo practitioners and small practices and they were doing very well.” However, with the shifts in medical practice environments and the increasing difficulty of maintaining a viable small practice, he was confronted with a crucial choice.
The Inevitable Crossroads
As the landscapes of medical practices evolved, so did the challenges faced by physicians. Small groups, despite their commendable tenacity, found it difficult to stay competitive from an overhead standpoint and negotiate insurance contracts with equal footing. The last five years saw physicians standing at an inevitable crossroads: either become an employee and sell your practice to a hospital or a large group, or expand by merging with more doctors in your specialty. Dr. Hale explains, “And there’s only so much you can do in a small group to stay competitive…you have to decide between becoming an employee and selling your practice…”
Pursuing the Route of Expansion
Dr. Hale and his group had a choice to make. And they chose not to sell, but instead to expand. The decision might have been fraught with hurdles and uncertainties, but they understood the importance of maintaining their autonomy, their ability to offer personalized care to their patients. He says, “But in our group, we decided it was better not to sell, but instead get bigger.”
And that’s when they came across the Advanced Urology Institute (AUI).
Joining Forces with Advanced Urology Institute
Taking their quest for growth and top-notch care to the next level, Dr. Hale and his group decided to merge with the AUI. This strategic move allowed them to not only augment their resources but also negotiate contracts from a more competitive pedestal.
The AUI, the largest urology practice in Florida, serves as a testament to the power of collective brilliance, a convergence of expert urologists, all dedicated to providing unparalleled care to their patients. It’s an institution that continues to imbibe the spirit of unity, growth and relentless pursuit of excellence — the same spirit that led Dr. Hale and his group to its doorstep.
Seeking Excellence with Advanced Urology Institute
Choosing to align with the Advanced Urology Institute has been an impactful decision for Dr. Hale’s practice. What began as a solitary journey in urology has now transformed into a collaborative endeavor, all thanks to a shared vision for excellence and dedication to patient care.
In the world of urology, the choice is clear. Join forces with those committed to innovation, community, and excellence. Like Brian Hale, MD, choose Advanced Urology Institute. As the largest urology practice in Florida, they are at the forefront of healthcare delivery, ensuring that their patients receive the best possible care in Palm Harbor, Tampa, and New Port Richey. Stand with Advanced Urology Institute, stand with quality care.
References:
- AUI. (2023, September 21). Mikhail Lezhak, PA C: Choosing AUI. AUI. https://www.advancedurologyinstitute.com/mikhail-lezhak-pa-c-why-you-should-choose-advanced-urology-institute/
- AUI. (2023, August 17). Brian Hale, MD: Urological Care with AUI. AUI. https://www.advancedurologyinstitute.com/brian-hale-md-elevating-urological-care-with-advanced-urology-institute/
- Watson, S. (2016, May 25). Faces of Healthcare: What Is a Urologist? Healthline; Healthline Media. https://www.healthline.com/health/what-is-a-urologist
- The role of a urologist. (2023, September 4). Healthdirect.gov.au; Healthdirect Australia. https://www.healthdirect.gov.au/urologist
- And, D. (2023, September 25). Urologic Diseases – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases
Mikhail Lezhak, PA C: Why You Should Choose Advanced Urology Institute
Key Takeaways:
- Advanced Urology Institute combines geo-strategic accessibility, in-depth expertise, cutting-edge technology and a personal, nurturing approach.
- The Institute has the best technology available to offer evidence-based, personalized care.
- The Advanced Urology Institute is committed to excellence, striving for better and offering the best available treatment for urological diseases.
 As you navigate through the complexities of health, the importance of personal, empathetic, and state-of-the-art care cannot be understated. Florida’s Advanced Urology Institute (AUI) stands at the forefront of patient-focused urological treatments, spearheaded by talented professionals like Mikhail Lezhak, PA-C.
As you navigate through the complexities of health, the importance of personal, empathetic, and state-of-the-art care cannot be understated. Florida’s Advanced Urology Institute (AUI) stands at the forefront of patient-focused urological treatments, spearheaded by talented professionals like Mikhail Lezhak, PA-C.
“My name is Mikhail Lezhak. I’m a physician assistant with Advanced Urology Institute in Daytona,” he begins, setting the tone for an intimate dialogue on an often-overlooked field of medicine. At the heart of this discussion is you. You are not just another patient on a long list, but an individual deserving of top-tier medical care. This simple yet transformative principle is at the core of the Institute’s ethos.
Why Choose Advanced Urology Institute?
The answer lies in the convergence of geographic accessibility, in-depth expertise, cutting-edge technology and a personal, nurturing approach. As Mikhail Lezhak notes, “We have locations in many places in Central Florida and not only.” This geo-strategically dispersed presence ensures that no matter where you are in Daytona, FL or the surrounding areas, quality urological care is never far away.
The Institute’s physicians, urologists and Physician Assistants, like Lezhak, bring to the table an unrivaled collective prowess. “We’re very knowledgeable,” he asserts, “and they [the physicians] can help you with any urological problems and treat any kind of urological disease if you have any. And as a PA, I can help them doing that.”
Unparalleled Technological Advancements
AUI impressively aligns human compassion with technological evolution. “We are equipped with the top-of-the-line technology and machines that help to evaluate patients thoroughly,” Lezhak explains, delineating how the Institute is always a step ahead in the evolving medical landscape.
Having the best technology at their disposal allows these capable professionals to offer the best available treatment to the patients. Evidence-based, personalized care is not an abstract concept here, but a daily reality, seamless in execution and delivered with earnest compassion.
A Holistic Approach to Urological Care
AUI’s approach is holistic and patient-centric. The journey from diagnosis to treatment and beyond is mapped out with the utmost sensitivity, taking into account each individual’s unique circumstances.
As Lezhak underscores, his role as a PA enables him to contribute meaningfully to this journey. In this intricate dance of medical intervention, the patient is always at the center, enveloped by a team of experts dedicated to their wellbeing.
A Commitment to Excellence
The largest urology practice in Florida, AUI, has carved out an irreplaceable niche in the landscape of urological care. It is not simply about the cutting-edge technology, the wide-ranging presence across Daytona, FL, or the team of accomplished urologists and Physician Assistants. It is about the commitment to excellence, the relentless striving for better, and the knowledge, as Mikhail Lezhak puts it, “that we can offer the best available treatment currently for urological diseases.”
Choosing the Advanced Urology Institute for your urological care is choosing unparalleled expertise, cutting-edge technology, geographic accessibility, and above all, a compassionate and personalized approach. Dedicate yourself to the best, because your health deserves nothing less.
References:
- AUI. (2023, August 17). Brian Hale, MD: Urological Care with AUI. Advanced Urology Institute. https://www.advancedurologyinstitute.com/brian-hale-md-elevating-urological-care-with-advanced-urology-institute/
- AUI. (2023, September). Samuel Lawindy, MD: Why Choose AUI. Advanced Urology Institute. https://www.advancedurologyinstitute.com/samuel-lawindy-md-why-choose-advanced-urology-institute/
- Watson, S. (2016, May 25). Faces of Healthcare: What Is a Urologist? Healthline; Healthline Media. https://www.healthline.com/health/what-is-a-urologist
- And, D. (2023, September 21). Urologic Diseases – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases
- Urology. (2015, April 7). Urology. Health Careers. https://www.healthcareers.nhs.uk/explore-roles/doctors/roles-doctors/surgery/urology
What Is BPH and How Can It Be Managed?
Understanding Benign Prostatic Hyperplasia and its Treatment🩺🔄What Is BPH and How Can It Be Managed? At Advanced Urology Institute.
Continue readingRolando Rivera, MD: Shockwave Therapy – Expert Insights and Opinions
Unveiling the Power of Shockwave Treatment🩺 Rolando Rivera, MD: Shockwave Therapy – Expert Insights and Opinions
Continue readingWhat Causes Bladder Stones and How Are They Treated?
Unveiling the Origins and Solutions! 🩺💎 What Causes Bladder Stones and How Are They Treated? Learn more at Advanced Urology Institute.
Continue readingHow Do Kidney Stones Form and How Can They Be Treated?
Unlocking the Mystery and Solutions! How Do Kidney Stones Form and How Can They Be Treated? Learn more at Advanced Urology Institute now.
Continue reading