Transforming prostate cancer care with the Da Vinci Robotic System. Our FL urologists utilize this advanced technology for precise, minimally invasive procedures
Continue readingAdvanced Urology Institute: Strategies for Kidney Stones Prevention
To reduce the risk of recurrence, here are some strategies for kidney stones prevention from Chad Bryan, a physician assistant in Largo, FL.
Continue readingChad Bryan PA-C: The Vital Role of Communication in Urology Care
Chad Bryan, PA-C, a physician assistant in Largo, FL talks about the vital role of communication in urology care.
Continue readingAdvanced Urology Institute: Addressing Sexual Dysfunction in Men and Women
The subject of sexual health can be difficult especially when talking about the sexual dysfunction in men and women.
Continue readingAdvanced Urology Institute: Advancing Urological Care with Immunotherapy
Advanced Urology Institute aims to provide the best quality of life for our patients, including advancing urological care with immunotherapy.
Continue readingThe Impact of Radiation Therapy in Urological Care
Our urologists in Naples and Largo, FL provides a foundation for understanding the impact of radiation therapy in the realm of urology.
Continue readingNicole Szell, DO: Elevating Quality of Life Through Urological Expertise
Dr. Nicole Szell, a urologist in Advanced Urology Institute in Largo, FL whos demeanor and urological expertise helps her patients be at ease.
Continue readingWhat are the treatment options for prostate problems according to Dr. Scott Klavans?
2 Effective Treatment Options for Prostate Cancer
Prostate cancer can be treated and managed in a number of ways. While the preference of the patient is given priority, it should be tempered with the advice of a trained urologist. A urologist can offer advice on what method is appropriate depending on the age of the patient, the patient’s family history and the natural progression of the disease. The patient also needs to be fully advised of the side effects of any form of treatment before agreeing to undergo the treatment. For any given case of prostate cancer, there are always at least two treatment options available.
1. Surgery
A patient with prostate cancer can choose to have the prostate surgically removed to clear the cancer from the body. The procedure is known as Radical Prostatectomy. It is most appropriate in cases where the cancer is localized and has not spread beyond the prostate. However, even when the cancer is localized, a urologist will determine the progression of the disease before recommending surgery. Low risk localized prostate cancer is unlikely to progress and a radical prostatectomy is unnecessary. On the other hand, when the cancer is aggressive and is likely to result in death if untreated, surgery is definitely the most appropriate choice.
Radical prostatectomy is recommended for patients under the age of 75 , or those with a life expectancy of at least ten years. This is because they are more likely to preserve their sexual and urinary functions after the surgery and they have a stronger chance of outliving any side effects the surgery might have.
2. Radiation Therapy
Radiation therapy, or radiotherapy is the use of radiation in high doses to kill malignant cancer cells or slow their development. Unlike radical prostatectomy, it can be used to treat localized prostate cancer and even advanced prostate cancer. It may be applied in combination with other treatment options such as hormone therapy. It may even be applied if a patient undergoes a radical prostatectomy but the procedure fails to eliminate the cancer fully or if the cancer recurs.
Radiation therapy can be administered externally or internally. When done externally, it is referred to as external beam radiation and is very much like having an X-ray. When administered internally, it is referred to as brachytherapy or internal radiation therapy. In this procedure, a radiation implant is placed inside the body near the affected organ. After a while, the implant ceases to produce radiation. The implant, however, remains in the body.
Both radical prostatectomy and radiation therapy are suitable treatment options and choosing between them may seem a little daunting. The professional opinion of a urologist can help by pointing out the finer points of each choice. The patient also may research the subject by reading up on the various options. There are many sites that offer reliable material on this subject.
For more information about treatment options for prostate cancer, visit the “Advanced Urology Institute” website.
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
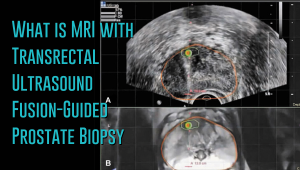 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
The Effectiveness of Erectile Dysfunction Treatments
Worried about your inability to get or maintain an erection? Stop worrying and visit your doctor for an open and honest chat. A urologist can help you find safe and effective treatment of erectile dysfunction that will enable you to approach any future dates with your partner with confidence. Urologists are experts in treating erectile dysfunction and other genitourinary issues, so do not be anxious about such a visit. In fact, you will be surprised to find that your doctor is probably seeing up to a half dozen men with ED every week.
Oral ED Medications
The first choice of treatment for ED is usually oral medications called phosphodiesterase inhibitors type 5 (PDEi-5). These drugs include the first-generation agents such as sildenafil (Viagra), vardenafil (Levitra) and tadalafil (Cialis), together with second-generation agents like mirodenafil (Mvix), iodenafil (Helleva), udenafil (Zydena) and avanafil (Stendra). With the drugs providing a normal, natural erection in 80-95 percent of men as long as there is sexual stimulation, they are the best option for many men with ED. They also deliver high efficacy rates and favorable safety levels.
Transurethral and Intracavernosal Injections
If you are unresponsive to oral drugs, your doctor will review your treatment and consider other options. The urologist may consider a transurethral injection with a drug called alprostadil. The doctor may go for this option if your penile nerves have been compromised and you need to bypass the neurological pathways responsible for an erection. Another option may be an intracavernous injection of papaverine, phentolamine, PGE1 or vasoactive intestinal peptide (VIP). The injections are a good treatment choice with 91-96 percent success rates and proven safety. These drugs may be combined for better efficacy.
Vacuum Constriction Devices
Vacuum erection devices also may be considered. But these are commonly offered to elderly patients who may only want occasional sexual intercourse. Younger men do not like these devices because of the unnatural feeling of the erections and the mechanical procedure necessary to produce the erections. You should discuss this option with your doctor and find out if the devices are ideal for you.
Surgical Therapies
When medical therapies fail, your urologist may recommend surgery. Surgical procedures are often the last option because of the cost, non-reversibility and invasiveness involved. There are two kinds of surgery for men with ED: penile prosthesis and penile revascularization. In penile prosthesis, the urologist inserts an inflatable or semi-rigid implant into the penis tissue. The success rate of penile prosthesis is 97 percent, but the implant must be replaced every 8-15 years. Penile revascularization is a surgical procedure to repair either venous ligation or arterial stenosis. Explore surgery with your doctor if the other options fail to work for you, but be sure to understand what is involved before you make a decision.
Non-Specific Interventions
Erectile dysfunction treatments may be accompanied by other interventions. For instance, psychotherapy is a noninvasive and highly effective intervention that is often combined with other therapies for a better success rate. Likewise, your urologist may recommend lifestyle modifications, such as increased physical activity, dietary changes, moderate alcohol consumption or a decision to stop smoking in order to improve your ED symptoms and minimize cardiovascular risk. If tests show that you have low testosterone, your doctor may recommend testosterone replacement therapy before you use ED-specific medications. If you are a younger, healthier man, testosterone therapy may just be what you need for enhanced sexual desire and harder erections.
At Advanced Urology Institute, we have established a multidisciplinary, compassionate and patient-centered approach to the treatment of erectile dysfunction. We prioritize the needs and expectations of our patients during treatment, educating them and providing a supportive environment that ensures shared decision-making. We also conduct meticulous follow-ups to identify any changes in the relationships, health and emotional status of our patients to optimize the efficacy of our treatments. If you are experiencing bothersome and embarrassing ED, visit one of our urologists for help. Get more information on the treatment of erectile dysfunction at the “Advanced Urology Institute” site.
Webb McCanse Becoming a Urologist
Becoming a Urologist
The opportunity to work in the Navy was very attractive to me. So I pursued medicine as a path to serving my country. With the United States
Navy taking care of my fees, I completed my medical school training at the University of Kansas and joined the University of Nebraska’s Medical Center for a six-year urology residency. Upon completion, I served in the United States Naval Hospitals of Pensacola and Guam, with sporadic assignments in Cuba and Okinawa, Japan. Following a satisfying naval service, I moved to Advanced Urology Institute.
Areas of Expertise
My extensive training exposed me to a number of advanced technologies and medical procedures. I am an expert in minimally invasive surgical procedures, particularly laparoscopic surgery and robot-assisted surgery for a wide range of genitourinary disorders. At AUI, I see patients with urologic cancers (bladder, penile, urethral and prostate), kidney stones, benign prostatic hyperplasia (BPH), overactive bladder and urinary incontinence, among other conditions. I no longer serve in the Navy, but I am still proud to serve my country by helping its citizens overcome some of the most painful and embarrassing conditions.
Job Satisfaction
Urology is a very interesting profession, with each day presenting new challenges. We educate patients on living healthy lives, achieving their goals and making informed decisions. The level of engagement with patients is just amazing. We get to know our patients, gain their trust and build enduring relationships with them. It is greatly satisfying to just be there for a person who is suffering but feeling embarrassed to discuss his condition. Then to be able to help him open up, discuss the symptoms freely and find relief just brings incredible joy. As a urologist, I am proud of my specialized role and am deeply contented, satisfied and fulfilled as a person.
Why Advanced Urology Institute
Advanced Urology Institute is a pool of like-minded and experienced professionals working through a collaborative, multidisciplinary, patient-centered approach to deliver the best possible care to patients. Our job is not merely to diagnose and treat, but also to help people be proactive and take control of their lives. We consider the different patient needs, offer tailored consultations and treatments, and are always there for our patients. I love working at AUI because it offers the best opportunity for me to serve my country through timely, safe and effective urological care to its citizens. For more information on urological services offered at AUI, visit the “Advanced Urology Institute” site.
Christopher Sherman Becoming a Urologist
The Long Path
Right from childhood, I have had a knack for helping people rise above their limitations. As a native of Florida’s Coral Springs I was often surrounded by people with various medical conditions who had few physicians to attend to them. I made up my mind early that I would pursue medicine to be able to make an impact on these lives. I got my undergraduate degree in health science at the University of Florida, then moved to the College of Medicine, Florida State University, for my medical school degree. After that I took a one-year general surgery training followed by a four-year urology residency at the University of Louisville in Kentucky.
Areas of Expertise
During my training, I became interested in medical technology and in advanced medical procedures. I not only honed my skills in minimally invasive techniques and robot-assisted surgery, but also mastered a number of specialized procedures such as laser surgery for BPH, Botox therapy for overactive bladder, interstim therapy for underactive and overactive bladder, and urethral slings for voiding dysfunction. Through my expertise as a urologist, I have been able to achieve my life’s dream of re-igniting the desire and joy to live in people facing their most uncomfortable, painful or lowest moments. As a urologist, I always feel a sense of peace and fulfillment after making a positive change in the life of a patient.
Job Satisfaction
As urologists, we work for long hours and often face stressful situations. But we take pride in our capacity to persevere and consistently deliver safe, timely and effective treatments. In fact, the challenges just help bring out the best in us and make our job even more interesting. We understand that to have the opportunity to help the sick is very rewarding. We also get to know our patients, win their trust and establish very close relationships. It is so satisfying to take care of patients and be able to make a difference in their lives.
Why Advanced Urology Institute
Every urologist yearns for a workplace that can bring out the best of their skills, talents and experiences and enable them to offer the best possible care. At Advanced Urology Institute, all administrative work has been centralized, allowing physicians to have enough time, tools and drive to collaborate, research, innovate and give the best possible care to their patients. AUI enables us to be in the company of other skilled, passionate, hard-working and creative people, making it easier for us to perform at our best and to take our careers to whatever heights we imagine. At AUI, urologists are living their dreams! For more information, visit the “Advanced Urology Institute” site.