Discover Unmatched Urological Care in Leesburg! Advanced Urology Institute Leesburg Office offers Exceptional Care. Book an Appointment Now!
Continue readingWhat is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
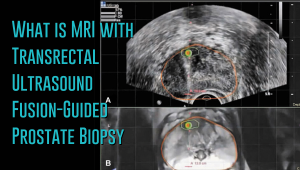 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Advanced Urology Institute – Urologists Working Together for You
Video: Advanced Urology Institute – Urologists Working Together for You
We believe that medical care is best delivered between an independent physician and a willing patient. When the physician is not in control, bad medicine (profit driven) results. [Read Full Article…]
Cryotherapy in Urology
Cryotherapy (also called cryoablation) does not require an incision. Instead, the elemental gas argon is directly administered with cryoneedles to freeze the targeted cancer cells. [Read Full Article…]
Dr Richard Roach – Prostate Cancer Treatment
Video: Dr Andrew Sher – Prostate Cancer Treatment
Surgery is uncommonly done for patients age 70 and over, as the gain in benefit does not counterbalance the increased risk. The operation is usually done through a lower abdominal incision, although some surgeons prefer the perineal approach, where the incision is made between the scrotum and rectum. [Read Full Article…]
Penile Prosthesis – Very High Satisfaction Rate
Video: Low Testosterone – Urologists Treat The Whole Patient
This procedure has a success rate of about 90%-95% five years after insertion. Most men rate the erection as shorter than their natural one. A penile prosthesis does not change the sensation on the skin of the penis or the ability to reach orgasm or ejaculate. Contact a urologist who knows this procedure. [Read Full Article…]
Low Testosterone – Urologists Treat The Whole Patient
Video: Low Testosterone – Urologists Treat The Whole Patient
Having low testosterone does not have to be an issue in your life; testosterone replacement therapy can help you regain your overall health. Before starting any medications, it is advised that you talk to your doctor. [Read Full Article…]
Becoming a Doctor – Realizing That I Wanted To Be A Urologist
Dr. Richard Roach became a board certified urologist on 1989. His specialties include plasma vaporization for BPH, treatment of female stress incontinence and penile prosthesis for ED. [Read Full Article…]
Advances in Medical Technology by Dr. Richard Roach
Urologist is a medical practice dedicated to the treatment of disorders and diseases related to the male and female genito-urinary organs, including the kidney, ureters, bladder, prostate and genitalia. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]
What is Erectile Dysfunction? by Dr. Richard Roach
A man may have Erectile Dysfunction if he had failed to have an erection, or may have inconsistent ability to achieve an erection and lastly he can only sustain an erection briefly. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]
Dr. Andrew Sher on Advances on Urological Technology
Advanced Urology Specialists is proud to serve our patients with the lifesaving da Vinci System. This revolutionary robotic-assisted surgical tool allows us to heal patients with greater precision than ever before. Contact a urologist who knows how to operate the da Vinci System. [Read Full Article…]
Why Dr. Andrew Sher Chooses Urology as His Field
After earning his medical degree at Emory University, Dr. Andrew Sher completed his residency at the University of Tennessee. Dr. Sher is an expert at minimally invasive ablative prostate cancer treatment, with interests in nutritional and complementary treatments. [Read Full Article…]
What is Erectile Dysfunction? by Dr.Andy Sher
Erectile dysfunction (impotence) affects approximately 30 million men. This common problem can be a sign of a health condition that needs treatment such as poorly controlled diabetes or cardiovascular disease. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]
Dr. Richard Roach’s Specialty – Cryotherapy
Cryotherapy (also called cryoablation) does not require an incision. Instead, the elemental gas argon is directly administered with cryoneedles to freeze the targeted cancer cells. Contact a urologist who knows the cryotherapy procedure. [Read Full Article…]
Dr. Andy Sher on Overactive Bladder
Incontinence is a medical condition resulting in the uncontrollable leakage of urine, also known as an overactive bladder. This leakage can happen because of a strong urge to urinate and an inability to prevent urination. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]