Advanced Urology Institute: Dr. Samuel Lawindy’s Expertise and Why Choose Us. Learn More Insights From Expert Urologists Now.
Continue readingDr. Samuel Lawindy Talks About How to Treat Urge Incontinence in Women
KEY TAKEAWAYS:
- Urge incontinence is a condition characterized by a strong, sudden uncontrollable urge to pass urine, which often results in urine leakage. It is often caused by dysfunction of the bladder or pelvic floor muscles due to factors such as pregnancy, childbirth, and hormonal changes around menopause.
- The treatment for urge incontinence often involves a combination of medications, such as anticholinergics and beta adrenergics, and behavioral treatments like bladder training, pelvic muscle exercises, biofeedback, or urge suppression. If medications don’t work, minimally invasive procedures may be recommended.
- At Advanced Urology Institute, prompt, reliable, and effective treatment is provided to patients suffering from urge incontinence, emphasizing that it is a treatable medical problem and should not be accepted as a normal part of aging.
At Advanced Urology Institute we see an increasingly high number of women presenting with urge incontinence. Urge incontinence is a condition where you are unable or have difficulty holding urine in your bladder long enough to reach the bathroom. And so, it is characterized by a strong, sudden uncontrollable urge to pass urine, which often results in urine leakage.
What are the signs that a woman has urge incontinence?
- Urine leaks associated with a sudden compelling desire to pass urine
- Strong urge to urinate frequently
- Changing multiple incontinence pads through the day
- Awkward leaks of urine that cause embarrassment
- Organizing life and activities around bathroom locations when in new environment
What causes urge incontinence?
Even though up to 50-percent of women may have urge incontinence at some point in their lifetime, roughly 10-20 percent experience extremely bothersome urge-related urine leakage.
Incontinence may occur as a separate condition, but in some women, it presents alongside other forms of incontinence due to an underlying medical condition.
Urge incontinence is often caused by dysfunction of the bladder or pelvic floor muscles.
Generally the dysfunction is due to:
- Pregnancy
- Childbirth
- Hormonal changes just before or after menopause
How is urge incontinence treated?
If you have persistent urge-related urine leaks, consider seeking a board certified urologist for a prompt diagnosis. During your visit, the doctor will take your medical history and conduct a complete physical examination focused on your urinary system, reproductive organs and nervous system. The doctor will also order various tests which will likely include an analysis of your urine sample.
If urge incontinence is diagnosed, your doctor will prescribe medications to relax your bladder and pelvic muscles as a way of relieving the symptoms. The medications may be used alone or in combination with behavioral treatments, such as bladder training, pelvic muscle exercises, biofeedback, or urge suppression.
The two major classes of medications used for urge incontinence are: anticholinergics and beta adrenergics.
The anticholinergic drugs include:
- Darifenacin (Enablex)
- Fesoterodine (Toviaz)
- Oxybutynin (Ditropan, Oxytrol, Gelnique)
- Solifenacin (VESIcare),
- Tolterodine (Detrol),
- Trospium (Sanctura).
The beta adrenergic medications include:
- Mirabegron (Myrbetriq)
- Vibegron (Gemtesa)
Your doctor may also recommend vaginal estrogen (creams, pellets or rings) as a form of estrogen replacement therapy to help you if the incontinence is due to menopause, particularly if the incontinence occurs alongside vaginal atrophy (dryness).
If medications don’t work, your urologist may consider minimally invasive procedures. A procedure such as percutaneous tibial nerve stimulation, electrical stimulation, sacral neuro-modulation therapy (Interstim), or Botox bladder injection may be recommended.
Prompt, reliable and effective treatment
At Advanced Urology Institute, we encourage patients to believe that urine leakage does not have to be a normal part of aging. Incontinence is a medical problem that can be treated effectively to reduce symptoms or eliminate the problem completely. So we strongly insist that no woman should tolerate or endure this kind of discomfort, especially when it is bothersome and is affecting their quality of life.
If you’re struggling with embarrassing urine leakage, please get in touch with us to schedule your consultation and find out how we can help you. At AUI, we offer some of the latest and best interventions in treating urological disorders. For more information on the diagnosis and treatment of urinary incontinence and other urologic disorders, visit the site “Advanced Urology Institute.”
TRANSCRIPTION:
So my name is Samuel Lawindy.
I’m a board certified urologist at Advanced Urology Institute.
So there is urgency and urgent incontinence for women.
That occurs when someone feels that they have the desire to go to the bathroom and they
can’t quite make it in time and then they’ll be leaking urine before they get there, wearing
multiple pads throughout the day, always aware of where the bathroom is and that commercial
everyone knows about got to go, go, go to the bathroom.
That’s urgent incontinence.
Very easily treated with medications and multiple different medications can be utilized.
If that doesn’t work, then there is some minimally invasive surgical procedures that can help you.
REFERENCES:
- “Anticholinergics: List, Side Effects, Uses, Warnings, and More.” https://www.healthline.com/health/anticholinergics
- “Vaginal atrophy – Symptoms and causes – Mayo Clinic.” 17 Sep. 2021, https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288.
- “Incontinence: Leakage, Causes, Diagnosis, Treatment & Prevention.” 23 Oct. 2020, https://my.clevelandclinic.org/health/diseases/17596-urinary-incontinence.
Can Dr. Samuel Lawindy provide treatment for large kidney stones?
KEY TAKEAWAYS:
- Percutaneous nephrolithotomy or nephrolithotripsy (PCNL) is a specialized procedure designed to remove larger kidney stones (2 cm or bigger) or complex stones, where minimally invasive procedures such as ureteroscopy and shock wave lithotripsy are not effective.
- PCNL is performed under general anesthesia with a tiny incision made in the back of the kidney, using ultrasound or fluoroscopy guidance, and involves breaking the stone into smaller fragments with a laser or ultrasound, which are then safely flushed out of the kidney.
- While PCNL carries some risks, such as injury to nearby organs, infection, and bleeding, it is generally a safe and effective minimally invasive procedure that provides immediate relief from symptoms and fast recovery times.
A kidney stone that is 2 cm or larger in size causes more severe symptoms. Unfortunately, for such a large stone, the usual minimally invasive procedures such as ureteroscopy and shock wave lithotripsy do not work.
So you’ll need a more specialized procedure called percutaneous nephrolithotomy or nephrolithotripsy (PNCL).
PCNL is a surgical technique designed to remove kidney stones located in the kidney or upper ureter, where shock wave lithotripsy or ureteroscopy are not effective. Also, it is the ideal procedure for stones that are too large.
How is PCNL performed?
With percutaneous nephrolithotomy or nephrolithotripsy, a tiny incision is made through the back of the kidney directly to where the stone is. To gain access to the exact location of the stone in the kidney or upper ureter, the surgeon relies on the guidance of ultrasound or fluoroscopy.
Once the stone is reached, the surgeon uses a power source, such as laser or ultrasound, to break the stone into smaller fragments. The resulting smaller pieces are safely flushed out of the kidney through an external tube or an internal stent.
Typically, your surgeon passes a nephroscope—a miniature fiber-optic camera—together with other small instruments through the incision and into the kidney area where the stone is located. These instruments allow the surgeon to see the stone and to then use high frequency sound waves to break it.
If the resulting pieces of the stone are removed via the tube, the procedure is called percutaneous nephrolithotomy (PCNL). But if the stone is broken up and removed by other means, the procedure is called percutaneous nephrolithotripsy (PCNL).
Depending on the position of the stone in the kidney, the surgeon will take 20 to 45 minutes to complete the procedure. The goal of the procedure is to remove all of the stone, so that no pieces are left to pass through your urinary tract.
When is PCNL recommended?
Percutaneous nephrolithotripsy or nephrolithotomy is used for:
- Larger stones, 2 cm in diameter or bigger
- Complex stones
- Lower pole renal stones, larger than 1 cm
- Irregularly shaped stones
- Removing kidney stones in people with infections
- Stones that have not broken up enough by SWL (extracorporeal shock wave lithotripsy)
- Kidney stones in individuals who are not candidates for ureteroscopy
Is the procedure safe?
Percutaneous nephrolithotomy does have risks but is generally a safe, effective minimally invasive procedure. Most often, it successfully removes larger kidney stones and results in immediate relief of symptoms.
During PCNL, a hole is created in the kidney that should eventually heal without other forms of treatment. However, since the procedure is done around the back or abdomen, it comes with a small risk of injury to other nearby organs, like the ureter, bladder, liver, or bowel.
Also, like other surgical operations, PCNL comes with some risk of infection and bleeding. And because all surgeries on the kidney have a relatively rare long-term risk of high blood pressure or reduced kidney function later in life, the procedure carries these risks and should be conducted by an experienced, specially trained urologist.
What is the recovery like after PCNL?
Percutaneous nephrolithotomy is done under general anesthesia. So after the procedure, you will need a short stay in hospital to be monitored before you can go home.
Often, an overnight stay in the hospital after the surgery is enough and you can go home the very next day. Recovery is fast and generally smooth. You should be off work for just a week.
Safe, successful PCNL
At Advanced Urology Institute, we consider percutaneous nephrolithotomy one of the most effective techniques for stones larger than 2 cm in diameter. From our experience, patients leave the hospital stone-free after the procedure and are usually completely freed from any stone-related symptoms.
At Advanced Urologist Institute, we have a talented and skilled pool of urologists that perform the procedure frequently. For more information on the diagnosis and treatment of kidney stones, visit the site “Advanced Urology Institute.”
TRANSCRIPTION:
So my name is Samuel Lawindy, I’m a board certified urologist at Advanced Urology Institute.
So if you have a large stone in the kidney, usually two centimeters or larger, minimally invasive procedures such as a ureteroscopy or shockwave will not work.
So a PCNL or long term is percutaneous nephrolithotripsy would work very well for that.
That is where the procedure goes through the back of the kidney, directly to where the stone is and we can break it up and pull those pieces out safely and it’s a one night overnight stay at the hospital and you go home the very next day and usually patients tolerate it very well.
It’s a good option for patients who have that stone, it’s important to recognize that it is done here and does not require a tertiary care center, we do take care of it here at this facility.
- “Percutaneous Nephrolithotomy (PCNL) – Johns Hopkins Medicine.” https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/percutaneous-nephrolithonomy-pcnl.
- “Percutaneous nephrolithotomy – Mayo Clinic.” 26 Apr. 2022, https://www.mayoclinic.org/tests-procedures/percutaneous-nephrolithotomy/about/pac-20385051.
- “Nephroscopy – Cleveland Clinic.” 27 Jan. 2021, https://my.clevelandclinic.org/health/treatments/16254-nephroscopy.
What are the different treatment options for kidney stones according to Dr. Samuel Lawindy?
KEY TAKEAWAYS:
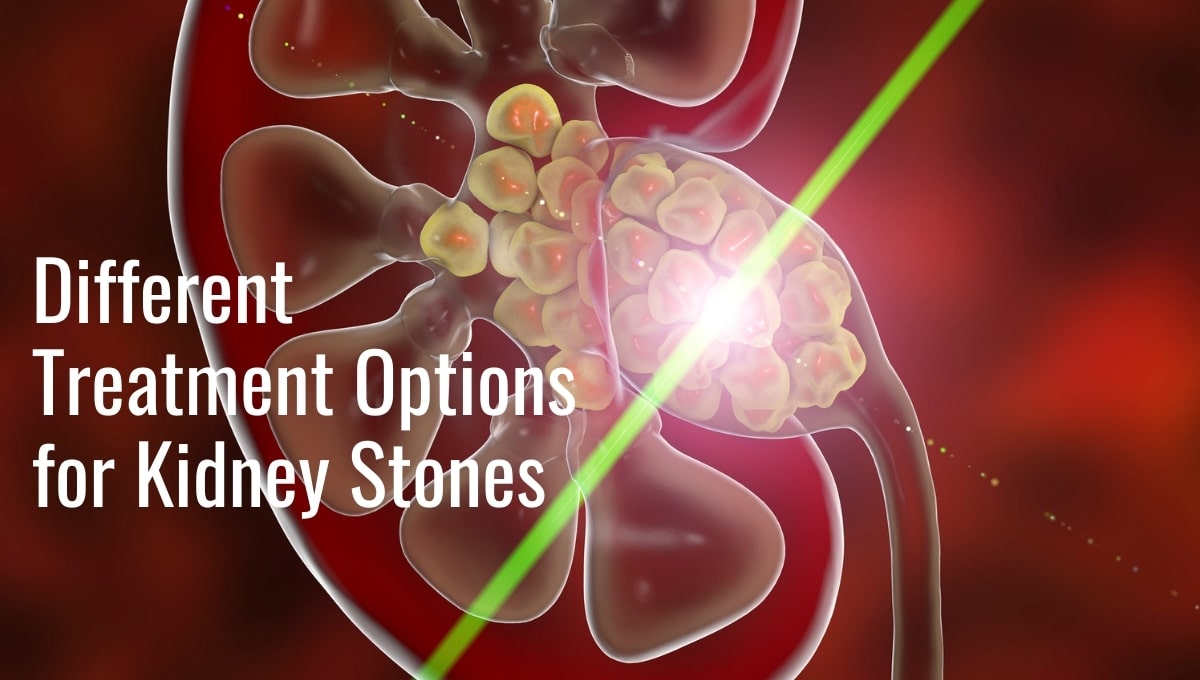
- Shock wave lithotripsy is a non-invasive and relatively pain-free treatment option for kidney stones, where shock waves are used to break the stones into small sand-like particles that can be passed naturally through urine.
- Ureteroscopy is a more invasive option for kidney stones, involving the use of general anesthesia and a long tool inserted into the urethra to find and remove the stones, with larger stones being broken up using a laser.
- For the largest stones that sit inside the kidney, a minimally invasive procedure may be required, where the urologist enters the kidney through the patient’s back to break the stone up or remove it through the incision, with recovery involving an overnight stay at the hospital.
Kidney stones are hard deposits of salts and minerals that form in the kidneys. They are a common and sometimes acutely painful occurrance that affects both men and women. Sometimes these stones can pass from the kidneys and become lodged in the tubes that connect the kidney to the bladder, called ureters. When this happens, kidney stones can become a big problem, causing painful symptoms that may require medical treatment.

Acute kidney stone symptoms include pain, nausea, vomiting and fever. When a patient experiencing an acute kidney stone episode sees their urologist, the first thing the urologist will do is insert a stint into the urethra. This will open it up and take pressure off the kidney, easing any pain that is present. With the pain subdued, the urologist can move on to assessing the kidney stone’s size and location in order to decide the best treatment option.
One of the best and newest treatment options is shock wave lithotripsy. For this treatment, shock waves are used to break the stone, or stones, into small sand-like particles. These much smaller particles are easier for the patient to pass naturally through their urine. Lithotripsy is a non-invasive and relatively pain free treatment option that is generally well tolerated by the patient.
Ureteroscopy is a slightly more invasive option for kidney stones. General anesthesia is used for this procedure in which a urologist uses a long tool inserted into the urethra to find and remove the kidney stone. In cases of larger stones, a laser is used to break up the stone so it can be scooped out with the tool. With this procedure, the urologist can see the stones as they are removed. Since this is a more invasive option than the shock wave lithotripsy, there is a slightly longer recovery time.
For the largest stones that sit inside the kidney, urologists may need to remove them through the patient’s back. Although still minimally invasive, it is the most invasive option listed here. The urologist will enter the kidney through the back and then either break the stone up or pull the whole thing out through the incision. Recovery for this procedure usually involves an overnight stay at the hospital and some mild pain that can be helped with pain medication.
Patients experiencing the pain and discomfort of kidney stones should be reassured that there are several established procedures for removing the stones. Dr. Samuel Lawindy of the Advance Urology Institute knows the importance of finding the right kidney stone treatment for each patient. For more information about kidney stones, visit the Advanced Urology Institute website.
TRANSCRIPTION:
So my name is Samuel Lawindy, I’m a board certified urologist at Advanced Urology Institute.
If you have an acute stone episode where you come in with a lot of pain, nausea, vomiting, fevers, the first step is to place a ureteral stent.
The stent will decompress the kidney, open it up, relieve the pressure, relieve any kind of infection that may be there, and take away the pain most importantly.
Once that’s in, then we have time to figure out what the next best option is in regards to treatment. So when talking about kidney stones, based on the size of the stone, the location of the stone, you can do anywhere from shockwave lithotripsy, where you break up the stone with sound waves, very minimally invasive, very well tolerated.
Next option is something called ureteroscopy, where we go in through the urethra from below all the way up to the location of the stone, and break it up with a laser.
And then we can pull those pieces out so it’s a little bit more definitive, in that we see the stone and remove it with an actual basket, however it’s a little more invasive so there’s a little bit more recovery time.
Lastly there is the larger stones that can sit inside the kidney that would be required to remove through the back, and that’s usually done in an overnight hospital stay, still relatively minimally invasive, but we go in through the back to the kidney, either break up the stone in small pieces and pull them out, or we can just grab the whole thing out and pull it out there.
For PCNL, recovery is usually an overnight stay at the hospital, there is a tube in the back that stays in place overnight, but then you go home with nothing, you go home with no tube in the back, no catheter from below, pain is relatively mild, but well controlled with pain medication.
REFERENCES:
- “Ureteroscopy: Purpose, Procedure, Risks, and Recovery – WebMD.” 20 May. 2021, https://www.webmd.com/kidney-stones/what-is-ureteroscopy.
- “Kidney Stone Treatment: Shock Wave Lithotripsy.” https://www.kidney.org/atoz/content/kidneystones_shockwave.
- “Large Kidney Stones – Treatments for Kidney Stones – Lithotripsy.” https://urologyaustin.com/general-urology/large-kidney-stones/.
What is Dr. Samuel Lawindy’s contemporary approach to treating overactive bladder with InterStim Therapy?
KEY TAKEAWAYS:
- InterStim therapy is a treatment option for patients with an overactive bladder, serious urine retention, or uncontrollable frequent urge to urinate, who have not responded to other treatments such as medication or physical exercises.
- The InterStim device is implanted in the upper buttock area through a minor surgical process called Sacral Nerve Stimulation Procedure, aiming to correct the communication patterns between the sacral nerves and the brain for better bladder control.
- The success rate of the InterStim device is high, with patients reporting relief from their symptoms almost immediately, but it is important to consult an experienced urologist to determine if a patient is a good candidate for the procedure.
InterStim therapy is a treatment option for patients with an overactive bladder, a serious case of urine retention or an uncontrollable frequent urge to urinate for reasons other than an overactive bladder. It gets its name from the InterStim, which is a small implantable device used to administer the therapy. There are other forms of treatment for overactive bladders, including medication and physical exercises. InterStim Therapy is used for patients who have failed to respond to the other treatments or who cannot undergo the treatments.
What is an Overactive Bladder?
 An overactive bladder is a condition characterized by sudden, frequent and uncontrollable urges to urinate. The patient feels the need to go to the bathroom numerous times during the day and the night. Sometimes, due to the uncontrollable nature of the urge, patients may have urine leakage, also known as urinary incontinence.
An overactive bladder is a condition characterized by sudden, frequent and uncontrollable urges to urinate. The patient feels the need to go to the bathroom numerous times during the day and the night. Sometimes, due to the uncontrollable nature of the urge, patients may have urine leakage, also known as urinary incontinence.
An overactive bladder may be caused by a neurological condition that interferes with the functioning of nerves that transmit messages between the brain and the bladder. Contributing factors can include diabetes, bladder complications such as tumors or stones, urine retention and an excessive intake of fluids.
InterStim therapy is focused on fixing the disconnect between the nerves in the brain and those that control bladder function.
The Procedure
The InterStim device is implanted in the upper buttock area through a minor surgical process called a Sacral Nerve Stimulation Procedure. Sacral nerves are located around the tailbone and regulate the operation of a person’s urinary function. Bladder movements are determined by the communication between the sacral nerves and the brain.
In patients suffering from an overactive bladder or urge incontinence, an InterStim device is implanted to enhance or correct the communication patterns between the sacral nerves and the brain, ensuring the person has full bladder control. Before the actual InterStim device is implanted, doctors place a temporary stimulator to observe how the patient responds. This helps to project what the efficiency of a permanent stimulator will be. If the patient does not respond at all to the temporary stimulator, then it would not help to implant a permanent one.
The success rate of the InterStim device is high, with patients reporting relief from their symptoms almost immediately. It is important to consult a urologist before having the device implanted because not every person may be a good candidate for the procedure. Since the surgery is a relatively delicate one, a patient should make sure to see an experienced urologist from a reputable institution, such as those from the Advanced Urology Institute. The staff of experts at Advanced Urology Institute can help with any questions, preparations and surgery. For more information, visit the Advanced Urology Institute website.
TRANSCRIPTION:
So my name is Samuel Lawindy, I’m a board certified urologist at Advanced Urology Institute.
For patients who have significant urge, urinary incontinence and urgency and frequency and medications have not quite treated that, there are a couple other options.
The inner stem is a nerve stimulation test that can not really test but a treatment for overactive bladder that it requires a small implantable device that goes into the upper buttocks that then stimulates the nerves to the spine that goes to the bladder to calm it down so that it gives you complete control over your urinary symptoms with no more leakage and more sleep throughout the night really.
And you don’t really have to think about it, it’s in there, it’s like a little pacemaker for the bladder, you control it with a little phone and you can adjust the settings that way.
REFERENCES:
- “Overactive Bladder | Polyuria – MedlinePlus.” 15 Sep. 2016, https://medlineplus.gov/overactivebladder.html.
- “InterStim for Overactive Bladder – Effectiveness for OAB.” https://www.urologysanantonio.com/interstim-for-oab.
- “Urge Incontinence: Causes, Symptoms & Treatment – Cleveland Clinic.” 5 Nov. 2021, https://my.clevelandclinic.org/health/diseases/22161-urge-incontinence.
What is the impact of low testosterone on men according to Dr. Samuel Lawindy?
KEY TAKEAWAYS:
- Low testosterone, or hypogonadism, can lead to reduced sex drive, shrinking testicles, low semen volume, and general fatigue in men.
- If left untreated, symptoms of low testosterone can increase in severity, potentially causing hair loss, infertility, low bone density, loss of muscle, and weight gain.
- Regular screening sessions for testosterone levels are important, and men experiencing symptoms should consult a trained urologist for diagnosis and treatment.
Testosterone is the hormone responsible for the development of the male sexual function. Besides being the main force behind a man’s sex drive and production of healthy sperm, testosterone also plays a role in the manufacturing of red blood cells and the distribution of fat in the male body as well as the regulation of muscle mass and bone density.
The production of testosterone drops gradually as men grow older and men over the age of 60 may develop symptoms of low testosterone. There are, however, instances where the production of testosterone slows down and falls below the required levels for reasons other than aging. Such men are said to be suffering from low testosterone. The level of testosterone can be measured through a simple blood test. In a normally functioning male, the level fluctuates between 300 ng/dL to 1000 ng/dL. If the level is below 300 ng/dL, then he may have low testosterone, also called hypogonadism.
Impacts of Low Testosterone on Men
 1. Reduced Sex Drive
1. Reduced Sex Drive
A drastic decrease in a man’s urge to have sex may point to low testosterone. Often this will be accompanied by a failure to achieve or maintain an erection, or erectile dysfunction. It is common for men mistakenly to attribute a reduced sex drive to aging. While it is true that the older you are the less interest you may have in sex, this is a gradual process that keeps pace with other bodily changes so when it happens, it is not that much of a surprise. It does not happen abruptly.
2. Shrinking Testicles
Testosterone causes the increase in size of the testicles and the penis during puberty. If the levels go down, it is to be expected that these organs may shrink. The testicles also may feel much softer.
3. Low semen Volume
Testosterone stimulates the production of semen, so low levels of testosterone inhibit the normal production of semen.
4. General Fatigue
Low testosterone levels also may cause a proportionate decrease in energy levels, leading to fatigue. This may be accompanied by a dislike for physical activity and movement.
If left untreated, the symptoms of low testosterone increase in severity and with time may cause hair loss, infertility, low bone density that can develop into osteoporosis, loss of muscle and a marked increase in weight because fat distribution remains unregulated.
The symptoms experienced by patients with low testosterone can mimic symptoms of other conditions. It is therefore necessary for one to undergo diagnostic tests with a trained urologist to determine the cause. Men also should schedule regular screening sessions where their testosterone levels are measured. And it is important to note that hypogonadism is treatable. The Advanced Urology Institute has a highly qualified staff of specialists that can offer a wide variety of treatment options as well as answer any questions. For more information, visit the Advanced Urology Institute website.
TRANSCRIPTION:
So my name is Samuel Lawindy, I’m a board certified urologist at Advanced Urology Institute.
Well low testosterone is a common issue that men may have. It is very important to be evaluated properly for low testosterone. There is a lot of lab values that can be obtained and a lot of information that can be obtained from the proper values and it is important to treat accordingly based on that number.
Not everyone should have testosterone. There are different ways to treat testosterone in regards to treating the hormone that provides testosterone in your body, sometimes blocking the hormone that converts testosterone to estrogen and it’s important to recognize that and treat that accordingly.
Low testosterone symptoms typically include fatigue, low libido, less desire for sex.
You can actually have weight gain, loss of muscle mass and some will actually have decreased outlook in life, somewhat depressed outlook.
Great, they feel wonderful.
If you treat them properly and the testosterone levels come up and they are doing well, tolerating medications well, then they live a normal healthy life.
They just need to be followed again, continually check the testosterone. It’s important to keep checking testosterone and they usually are very happy with the results.
REFERENCES:
- “Will Testosterone Rev You Up or Stall You Out? – WebMD.” 14 Apr. 2016, https://www.webmd.com/men/features/will-testosterone-rev-you-up.
- “Reproductive Hormones | Endocrine Society.” https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/estriol.
- “Testosterone: Functions, deficiencies, and supplements.” https://www.medicalnewstoday.com/articles/276013.
Dr. Samuel Lawindy: How Prostate Cancer Is Diagnosed
The prostate gland is the part of the male reproductive system that produces seminal fluid. Prostate cancer is the type of cancer that affects this organ. It is the most common cancer in men, with men over the age of 50 being at the greatest risk. It usually does not manifest symptoms in its initial stages. This is unfortunate because it means prostate cancer may not be detected until it is more advanced. Even when it does present symptoms, they might resemble other conditions such as an enlarged prostate. For this reason, before one concludes that they have prostate cancer, it is necessary that they first undergo the specific tests geared toward detecting it.
Diagnosing Prostate Cancer
There are two preliminary tests for prostate cancer. These are:
1. PSA Test. This tests for an antigen produced by and specific to the prostate. It is normal for the antigen to occur in small quantities. An unusually high level of PSA, however, may indicate the presence of prostate cancer or some other inflammation of the prostate.
 2. Digital Rectal Exam. This is very commonly used in prostate screening exercises. The doctor inserts a finger into the rectum and physically examines the prostate. If the doctor detects something unusual in the shape, mass or texture of the prostate, then there may be further tests to determine what the problem is.
2. Digital Rectal Exam. This is very commonly used in prostate screening exercises. The doctor inserts a finger into the rectum and physically examines the prostate. If the doctor detects something unusual in the shape, mass or texture of the prostate, then there may be further tests to determine what the problem is.
The two tests are not conclusive. They simply inform the urologist that something might be wrong and that the patient needs further examination. In order to test for cancer of the prostate specifically, the following procedures may be done after either of the initial tests.
A. A biopsy. A prostate cancer biopsy involves the use of a very fine needle inserted through the rectum to collect tissue from the prostate. The tissue is then tested for cancer.
B. Transrectal ultrasound. The doctor inserts a small probe in the rectum. The probe produces high frequency sounds that bounce off the prostate, producing an image of the prostate that can be projected on a screen and observed in greater detail.
C. MRI Fusion biopsy. This combines an MRI and the transrectal ultrasound to produce a clearer image of the prostate. It gives a better view of the part of the prostate that is affected. If a biopsy is to be performed later, it provides a picture of the precise area where tissue should be tested.
Early detection of prostate cancer improves the chances of successful treatment. It is important for men starting about age 50 to have regular screenings so that any cancer can be detected early. Seek out experienced and certified urologists, such as those on staff at the Advanced Urology Institute, to discuss any concerns and set up screening tests. Such examinations should be a regular part of a man’s health care.
For more information, visit the Advanced Urology Institute website.